
One year into program, we survey physicians about experience
CPSO’s Quality Improvement (QI) Program is getting positive reviews from those physicians who have participated in the self-directed learning program, with many reporting that participation has been key to helping them identify areas of improvement.
With the program in operation for a year, CPSO surveyed 530 physicians as to their experience in the program. The survey results found that:
- 75% of respondents took 16 hours or less to complete the QI program.
- 82% found the time to complete the QI program to be somewhat reasonable or very reasonable.
- 90% reported that their peer provided them with useful feedback about my practice.
- 86% reported that completing the Practice Improvement Plan was a “valuable part of my quality improvement effort.”
More than 380 physicians reported on the impact the program will have on their practice going forward. The most frequent answers were better condition management, better records practice and better practice management.
“We have had more than 2,000 physicians engage in the program and overwhelmingly, physicians who have completed the program have described it as a worthwhile, rewarding experience, even those who were skeptical at the outset,” said Dr. Mary Manno, a Medical Advisor with the program.
In 2020, CPSO launched its Quality Improvement Program for all physicians in Ontario. In transforming our approach we’ve moved from a single point in time assessment model to a proactive approach.
CPSO's suite of QI tools are designed to allow Ontario physicians to engage in self-reflection and practice improvement while meeting their quality requirements in five-year cycles.
The two QI Program streams at the CPSO align and fulfill our QI requirements. In addition, physicians participating in a CPSO Quality Improvement Program are eligible to claim CPD credits through the CFPC or the Royal College Maintenance of Certification program. This new program replaces our existing random peer assessment program for those under age 70. Those invited to participate in the QI program always have the option to defer for one year. And if there are other barriers for physicians in participating in the program, we want to hear about it so we can help.
The program is operated through an online Learning Management System, developed by the CPSO. Each learning module has been tailored to fit our new philosophy: self-directed physicians reflecting on their own delivery of health care and looking at data about their practices in relation to their peers and the associated standards of practice. These activities include chart review, peer feedback, setting goals, and outlining a plan for practice improvement. This process allows us to connect with more physicians, more regularly, in a more meaningful way - creating the conditions most favourable to ensuring their success at all stages of their career.
“I am confident that widespread use of the quality improvement skills embedded in the CPSO’s QI Program will result in significant benefits to patients, providers, their staff and, ultimately, the health-care system itself, said Dr. Manno.
The core principles for our QI Program are:
- A philosophy of assessment that focuses on continuous improvement
- Use of a platform that supports and integrates with physician needs and practice demands
- A proactive approach that facilitates interaction and self-reflection and strengthens practice
Select QI Survey Results
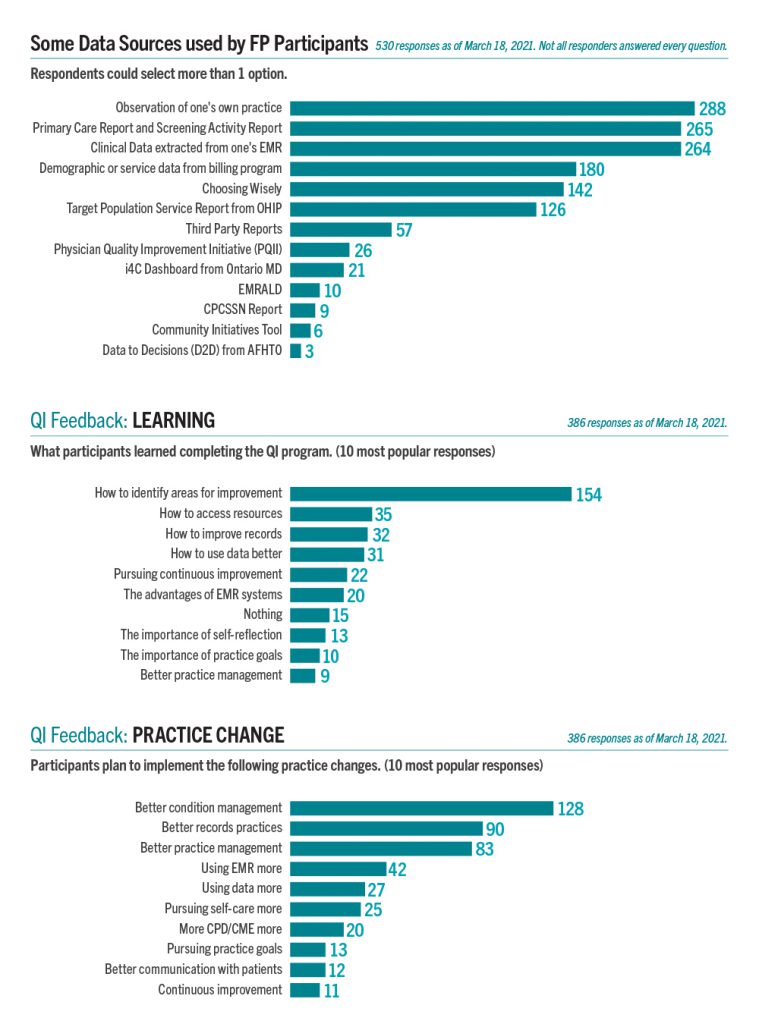
Some Data Sources Used by FP Participants (530 responses as of March 18, 2021. Not all responders answered every question)
Respondents could select more than one option.
The top five data sources used were: observation of one’s practice (288); primary care and screening activity report (265); clinical data extracted from one’s EMR (264); demographic or service data from billing program (180); and Choosing Wisely (142).
QI Feedback: Learning (386 responses as of March 18, 2021)
What participants learned completing the QI program. (10 most popular responses)
The top 5 things participants learned completing the Qi Program: how to identify areas of improvement (154); how to access resources (35); how to improve records (32); how to use data better (31) and the importance of pursuing continuous improvement (22). Other responses in descending popularity were the advantages of EMR systems (20); nothing (15); the importance of self-reflection (13); the importance of practice goals (10); and better practice management (9).
QI Feedback: Practice Change (386 responses as of March 18, 2021)
Participants plan to implement the following practice changes. (10 most popular responses)
The top five things practice changes participants plan to implement: better condition management (128); better records practice (90); better records management (83); using EMR more (42); using data more (27). Other responses in descending popularity were pursuing self-care more (25); more CPD/CME more (20); pursuing practice goals (13); better communication with patients (12); and continuous improvement (11).
















